I’m one of about 400 lucky people in Canada who get this surgery every year

This piece is written in the first person.by Harry Forestell, who has Parkinson’s disease and is the host of CBC News New Brunswick at six. He draws on his own experiences with the disease.
My new party trick is a great way to get people’s attention.
It gives a clear picture of how my Parkinson’s disease was before and after I got treatment. proof of how much can be done when you poke around in your head.
Deep brain stimulation (DBS) is the name of the treatment. It involves putting thin electrodes into the brain, where they send out small pulses of electricity. When these pulses are kept on just the right part of gray matter, they stimulate parts of the brain that control the signals that go to your muscles. In the brain’s engine room, the basal ganglia, signals are sent to the body to tell it to do things like speak, swallow, walk, and touch. When these messages don’t get through or when the instructions get mixed up, the body can act in a cruel way. Hands shake uncontrollably, legs shake, walking gets harder and harder, and it’s hard to even swallow.
All of these are early signs of Parkinson’s disease, but it is not the only thing that can happen.
More than 84,000 Canadians have symptoms of Parkinson’s disease.. The number of Parkinson’s cases in Canada is expected to double between 2011 and 2031.
Parkinson’s is a long-term disease that doesn’t kill people. You will die, as neurologists will often tell you.with Parkinson’s, not fromParkinson’s. Even though this is true, it doesn’t really show how the disease makes people lose control of their own bodies in a slow, sneaky way.
I’ve always been interested in stories like this one about medicine. I was a medicine and science reporter for a few years, and one of the stories I wrote about was the panic in the U.K. over mad cow disease. I did radio shows about how the brain grows and ages.
I had no idea that one day I would be writing about my own brain disorder.
A diagnosis that was both shocking and a relie
The day I found out for sure that I had Parkinson’s disease was both a relief and a shock.
It was 2015, and my wife Jenny and I had been going back and forth between hope and despair for the past two years. My Fredericton neurologist, Dr. Eva Pniak, who was patient and persistent, thought I had Parkinson’s disease. However, she also thought that the problems I was having walking and with my trembling hands could be caused by a condition calledessential tremor.
She sent me to a specialist in Toronto, who gave me a clear diagnosis.
At 53, I had Parkinson’s.
The basal ganglia are in charge of almost everything the body does, from jumping out of a tree to dancing the tango. With the help of a neurotransmitter called dopamine, these orders are sent at the speed of light through nerve networks. Movement disorders like Parkinson’s are caused by a drop in the number of cells in the brain that make dopamine. No one knows why this happens yet.
It’s a simple equation: no dopamine, no movement.
With Parkinson’s, these dopamine cells start to die off slowly, years before the first signs of the disease show up. Scientists don’t know why this happens or why they can’t stop or slow it down.
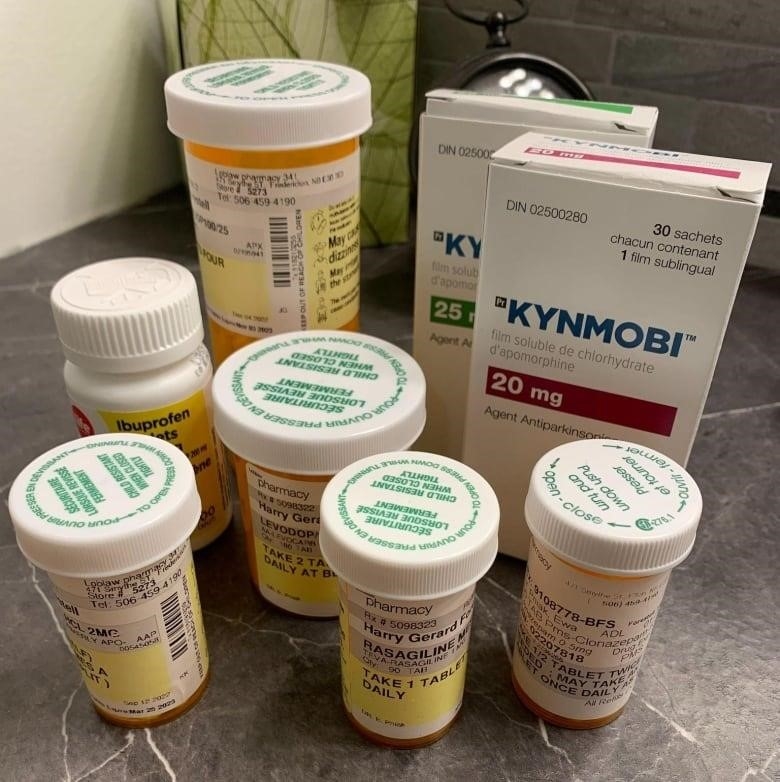
With a drug called levodopa, doctors can replace some of the lost dopamine, but it has a side effect called dyskinesia, which is sudden, uncontrolled muscle movements in the arms and upper body that make a twisting, writhing motion. Dyskinesia gets worse as doctors give more levodopa to stop Parkinson’s tremors.
Patients’ lives will be better because of it
Neurologists have been trying out DBS for nearly 40 years to treat Parkinson’s and other movement disorders. The U.S. Food and Drug Administration gave DBS the green light to treat Parkinson’s disease in 1997.
Since 2012, Canadians have been able to use the procedure.Less than 400 people a year get DBS. in Canada.
Why aren’t there more? The simple answer is that it is a treatment that requires complicated brain surgery done by highly trained teams of surgeons and a lot of care afterward.
Watch: How deep brain stimulation can help people with Parkinson’s deal with its debilitating effects
Dr. Tony Lang is in charge of the Movement Disorders Clinic at the Western Hospital.a world-leading centre for deep brain stimulation.
“The skill of the surgeon is very important,” he said.
“You need an experienced surgeon who knows how to do the procedure and where to put the electrodes.” “But after the surgery, you need to know how to program and adjust the stimulators, as well as change the doses of the medicines, which usually change after the surgery,” he said.
“So, it’s a very complicated procedure that takes a team, and after the surgery, the neurologist and nurses do a lot of the work to make sure the responses are the best they can be.”
Lang says that it is a process that needs help from provincial governments. The payoff is a treatment that can make a big difference in how well Parkinson’s patients can live.
“The Ontario government has seen how important it is,” Lang said, adding that he feels lucky to have a team of expert neurosurgeons, neurologists, nurses, and others to help patients.
“The government saw how important this method was and gave us what is called “volume-based funding,” which lets us work with a much larger number of people than most centers.”
My own story is a clear example of how DBS can help some people with Parkinson’s feel better.
Holes in my hea
When I went to Toronto Western Hospital on September 30, 2022, I knew what was going to happen, but I didn’t know what it would feel like or how it would sound.

I knew that someone was going to drill a hole in my head before the day was over. There’s at least one. Possibly two.
I was told by people I could trust that the drilling would sound like an airplane taking off. More like taking off in a Concordeinside my head!
Before surgery, I had a metal structure bolted to the top of my head that looked like a square lamp shade on top of a lamppost.
This was supposed to keep my head still during the MRI scan and the more delicate process of skewering my brain without hurting any of the important parts.
There was a lot going on in the operating room as half a dozen surgeons and nurses got ready for the procedure. My head frame was bolted to the surgical table, and plastic sheets were put over me to make a clean place for the skull opening.
Drilling two holes in my head about the size of nickels was just as loud as I had been told. But there was no pain; I just felt pressure.
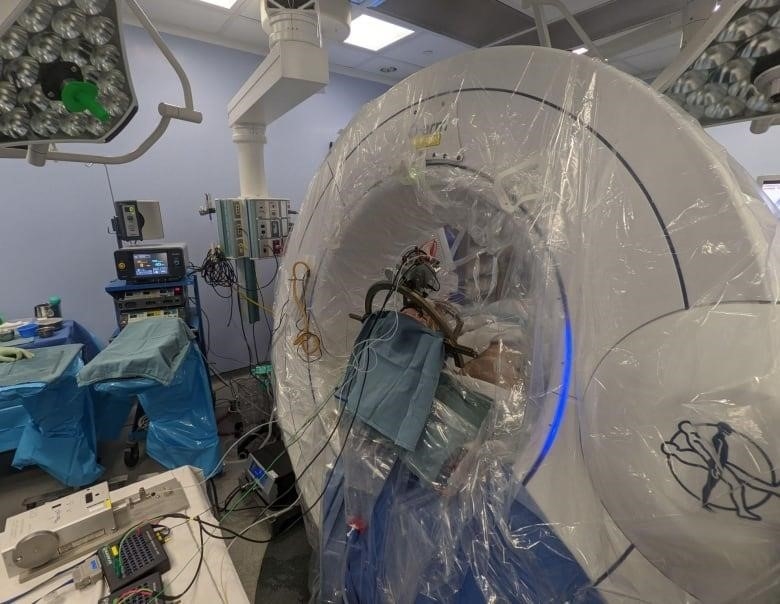
In the back of the room, a group of medical IT experts sat in front of computer screens, ready to track where the probes needed to go in my brain and give feedback and directions.
All of this I know because I was awake, wide awake, for the whole six-hour surgery. As a patient and the child of a hospital worker, I have spent a lot of time in hospitals. As a reporter, I’ve written about a lot of medical stories. So, instead of being afraid, the thought of this procedure made me curious. What would you think? What would be different? How would it go?
A strange experience indee
The surgical suite had the usual office noises going on. As I asked the surgeons questions about what was going on, we talked in a friendly way. In the background, I could hear a steady staccato, like the sound of a Geiger counter. This showed that my brain was still working.
Clicks coming from a loudspeaker made each busy cell seem even busier.
It was weird to have someone poke around in your head.

It didn’t hurt because the brain doesn’t have pain sensors. But as the probes moved into place, there were signs that let me know what was going on. Most often, my arm or leg would feel tingly, which was a sign that the electrodes were being carefully threaded through my brain to reach the basal ganglia.
Along the way, they asked me if I could recite the days of the week, the months of the year backwards, skipping every other month, and the order of prime numbers up to the fifth integer.
Once the probes were in place, the wiring and other hardware could be put in. For this part of the surgery, I had to be put to sleep with an anesthetic. Both probes are connected to wires that go through the skull and under the skin behind the ear, down the neck, over the clavicle, and then into a battery-powered pulse generator that sits just under the skin of the chest. This device is similar to a pacemaker. Even though the surgery has the usual risks, like infection, bleeding, stroke, and heart attack, side effects are rare.
A shocking conclusion
So, does it work?
Well, you can watch the video above to see the party trick I’ve been bragging about. Choose for yourself.
Here is how it works.
Once the electrodes are in the brain, they are controlled by a pulse transmitter and a modified cellphone to send the right amount of electrical stimulation.

The phone has an app that controls how often the basal ganglia are stimulated by electricity. The stimulator is set to send out regular electrical pulses, day and night. Somehow, these electrical pulses interrupt or override the jumbled neural instructions that are a sign of Parkinson’s.
I can walk normally all of a sudden. No shaking is happening. The annoying symptoms of dyskinesia, which I described above, seem to be going away.
Watch: Before getting DBS in September 2022, Harry Forestell told his audiences what he was going to do:
Regaining control of motor functions is a miracle, but it won’t work for everyone with Parkinson’s. DBS is not right for people with other health problems. It helps the most with motor symptoms in people who respond well to levodopa. When it works in those situations, it means that the drug and its side effects will be used less.
I’ve been able to cut the amount of medicine I take in half, and after four months off, I just went back to work. I sleep well, and even though I still get tired quickly, my mood has gotten better.
Parkinson’s will keep following me around for the rest of my life. DBS might give me another 10 or 15 years without tremors stopping me, but they will probably come back at some point as they get stronger. There are some sneaky side effects of Parkinson’s that DBS can’t fix.
But for now, it seems like the disease is locked up.
On a leash.
I can hear it barking, but it can’t bite me right now.
Do you have a compelling story about yourself that can help others understand or learn something? Here’s More information about how to sell to us.
