
A commission has given provincial and federal governments until May 1 to come up with a plan
The final report on the Nova Scotia mass shooting backs up what friends, neighbors, and family members of those killed in April 2020 have been saying for years: the province failed them and they are still dealing with a “public health emergency” because their mental health needs aren’t being met.
The Mass Casualty Commission’s long report came out last week. It says some harsh things about the situation in Colchester, Cumberland, and Hants counties in Nova Scotia.
The commissioners wrote, “Given the long-term effects of unmet support needs after mass violence, we call for this situation to be treated as a public health emergency.”
They gave the provincial and federal governments until May 1, 2023, to come up with and pay for a plan to deal with the problem. It’s the first benchmark of all 130 recommendations in the report.
“There is a difference. You have to wait months to see a psychiatrist or get into hospital programs for mental health that don’t cost money “Erin MacKinnon, who lives in Portapique, N.S., said this.
“It’s really hard to get help when you need it, and you can’t get it. I think that’s a big problem right now.”

On April 18 and 19, 2020, 13 people were killed in a small town in Colchester County. The shooting spree began in Portapique when the gunman attacked his partner. He killed nine more people the next day while pretending to be an RCMP officer and driving south across the province.
Even though support centers were set up right away in Portapique, Shubenacadie, Masstown, and Wentworth to help people find help, residents and families of victims told the inquiry that they were only given lists of psychiatrists and other professionals. Then they would find out that some therapists weren’t taking new patients or that they had to drive more than an hour to Halifax to get help.
The commissioners wrote that “the extent of unmet need cannot be measured” because there hasn’t been a needs assessment and the services that have been given haven’t been evaluated.
Two of the centers, in Portapique and Wentworth, stayed open much longer than planned, until January 2021. But MacKinnon said that the “denial process” was long because of the terrible things that had happened and because COVID-19 kept people from talking to each other.
MacKinnon said, “Once we started talking to our friends and neighbors in person and seeing things for ourselves, it really started to sink in and hit us.”
Then, a neighbor named Andrew MacDonald came to her door with the idea of doing something to help the community move forward, MacKinnon said, and their local “build-up” project got started.
Because of this, Portapique has a new playground and is building a new community center. MacKinnon said that the project has given her something positive to focus on, which has been “healing” for her. Their group recently got a grant to offer mental-health programs in the area.
“That gives us a chance to help people right here who need it,” MacKinnon said.
Still, she said that one idea won’t be enough to solve the problem.
‘We need more
“We need more, which is a sad thing to say. We’re happy with what we’re getting, but it needs to be more “MacKinnon said. “This is a battle we will always have to fight.”
In the Share Your Experience online survey, people wrote to the commission to talk about how the mass shooting affected them. Many of these responses were shared in the report.
One person wrote that they were disappointed that no new money had been put toward hiring more guidance counselors or school psychologists, who are usually in charge of more than one school.
“From what my son has told me, I know that our community has more kids who need mental health care than there are staff to treat them. This is very bad, “they put words on paper.
“If the deadliest mass shooting in Canadian history isn’t enough to make a region invest in mental health care, what needs to happen before a community’s youth get more money to help them?”

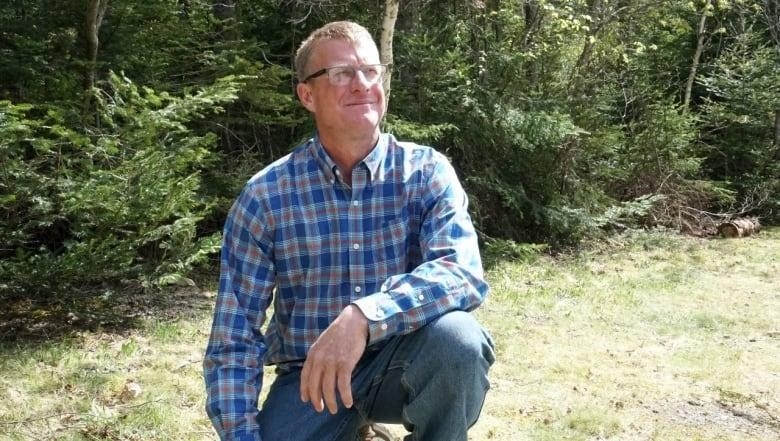
Laureen Rushton, who lives a 30 kilometres east of Portapique in Belmont, N.S., has been echoing the call for better resources. Lucas, her 18-year-old son, died in May 2021 of what she thinks was an accidental overdose. He had been sick mentally and had been struggling. She has said her son tried accessing mental-health services at least 50 times in the five years before his death.
Like many other people in the area, Rushton’s family had ties to some of the April 2020 shooting victims. She had taught at Debert Elementary School with Lisa McCully, knew Joy and Peter Bond, and Lucas had been in Emily Tuck’s class.
“After the shooting, we looked for him because it affected him and because he knew Emily and Lisa. They were pretty good friends, and it was hard for us to find a counselor “Rushton said.
Three years later, there is still not enough permanent mental health support in the community, Rushton said. He compared the province’s recent offer of a free one-hour counseling session to putting a Band-Aid on a surgical cut.
She has instead been trying to get the province to open walk-in mental health clinics that are separate from emergency rooms.
Rushton said that she totally agrees with the report’s assessment of the emergency.
“It’s my life. My son died because he wasn’t able to get the help he needed. Neither is he the only one, “Rushton said.
Leon Joudrey, a 54-year-old man from Portapique, died in November, just a few weeks after he met with the Mass Casualty Commission and others who had been hurt by the violence in a small group. Lisa Banfield, who was married to the gunman, ran to Joudrey for help early in the morning of April 19, 2020.
Joudrey talked at the time about how hard it was to figure out how to use the mental health system right after the shootings.
“When you’re shaking every day and someone tells you to wait three weeks for help, it doesn’t help much,” Joudrey told the commission. “It’s like dialing 911 and getting a recording.”
Joudrey said that since the shootings, he had spent most of the last two and a half years away from his property, which he was having trouble selling. Instead of living in the area where so many people had died, he stayed in a small cabin in the woods.
Friday, CBC contacted the Nova Scotia Health Authority about the lack of mental health resources in these counties. If they respond, this story will be updated.
Brian Comer, Nova Scotia’s Minister of Addictions and Mental Health, said on Friday that he is “committed to reviewing all of the recommendations” and that he will have more to say in the next few days.
Comer said, “We’ll definitely work with our federal colleagues to make things better for everyone in Nova Scotia, and I’ll work very hard on this file going forward.”

When asked about hiring more school psychologists for the three affected counties, Comer said that there are other programs for kids, like SchoolsPlus, but that the ratio of clinicians in the school system is “certainly something we can look at.”
The commissioners also recommended that federal, provincial and territorial governments develop a national action plan to better integrate preventive and supportive mental-health care into the health-care system to ensure greater access to these services “on an equal level as physical healthcare.”
Also, their report suggests that the Nova Scotia Health Authority work with community-based health organizations in the affected areas to come up with a public education campaign about grief, loss, trauma, and coping.
- The Nova Scotia mass casualty investigation was covered in full by CBC.
The report said that these campaigns to raise awareness should include ongoing education in schools and should be thought of along with existing programs. For example, employers might have to have them as part of programs for workers’ compensation.
The commissioners also say that Health Canada should work with the provinces and territories, as well as experts, to come up with a national policy for providing health and social support services to people and communities most affected by mass casualty events.
The report said that the national policy should include a team of experts from different fields who can be called in within 24 hours to help local service providers set up a support plan right away after a mass casualty.
MORE TOP STORIES
